Pacemakers regulate slow or irregular heartbeats by sending electrical impulses to maintain a steady rhythm, while Implantable Cardioverter Defibrillators (ICDs) monitor for dangerous arrhythmias and deliver shocks to restore a normal heartbeat if needed. Understanding the differences between these devices can help you make informed decisions about your heart health; read on to explore their unique functions and benefits.
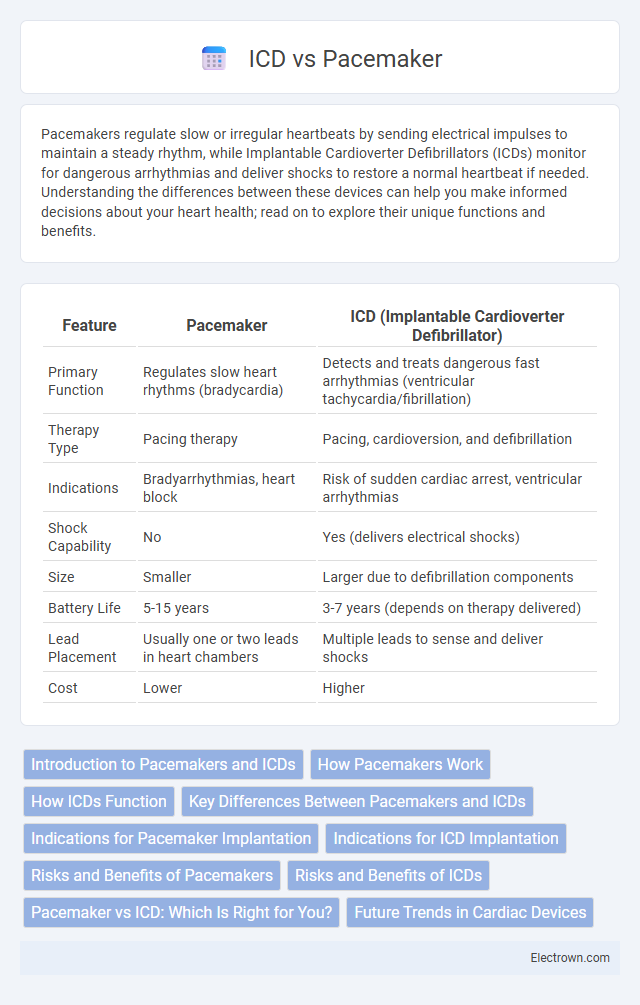
Table of Comparison
| Feature | Pacemaker | ICD (Implantable Cardioverter Defibrillator) |
|---|---|---|
| Primary Function | Regulates slow heart rhythms (bradycardia) | Detects and treats dangerous fast arrhythmias (ventricular tachycardia/fibrillation) |
| Therapy Type | Pacing therapy | Pacing, cardioversion, and defibrillation |
| Indications | Bradyarrhythmias, heart block | Risk of sudden cardiac arrest, ventricular arrhythmias |
| Shock Capability | No | Yes (delivers electrical shocks) |
| Size | Smaller | Larger due to defibrillation components |
| Battery Life | 5-15 years | 3-7 years (depends on therapy delivered) |
| Lead Placement | Usually one or two leads in heart chambers | Multiple leads to sense and deliver shocks |
| Cost | Lower | Higher |
Introduction to Pacemakers and ICDs
Pacemakers and Implantable Cardioverter Defibrillators (ICDs) are advanced cardiac devices designed to regulate abnormal heart rhythms. Pacemakers primarily address bradycardia by delivering electrical impulses to maintain adequate heart rate, while ICDs detect and correct life-threatening arrhythmias such as ventricular fibrillation through pacing or defibrillation shocks. Both devices are implanted subcutaneously and use leads positioned in the heart to monitor cardiac activity and provide timely intervention.
How Pacemakers Work
Pacemakers regulate heart rhythm by sending electrical impulses to the heart muscles, ensuring timely and adequate heartbeats, especially in cases of bradycardia. They consist of a pulse generator and leads that detect the heart's electrical activity and deliver impulses when the heartbeat is too slow or irregular. This helps maintain an effective heart rate and improves blood circulation throughout the body.
How ICDs Function
Implantable Cardioverter Defibrillators (ICDs) continuously monitor your heart rhythm and deliver electrical shocks to correct life-threatening arrhythmias, such as ventricular tachycardia or fibrillation. Unlike pacemakers that primarily regulate slow heartbeats by providing pacing pulses, ICDs detect dangerously fast rhythms and restore normal rhythm by defibrillation or anti-tachycardia pacing. This dual functionality makes ICDs critical in preventing sudden cardiac arrest in high-risk patients.
Key Differences Between Pacemakers and ICDs
Pacemakers primarily regulate slow or irregular heartbeats by sending electrical impulses to maintain a steady rhythm, while Implantable Cardioverter Defibrillators (ICDs) detect and correct life-threatening rapid arrhythmias by delivering shocks to restore normal heartbeats. Pacemakers are typically used for bradycardia and conduction disorders, whereas ICDs are crucial for preventing sudden cardiac arrest in patients at high risk of ventricular tachycardia or fibrillation. Your choice between these devices depends on the specific heart rhythm disorder and risk profile determined by your cardiologist.
Indications for Pacemaker Implantation
Pacemaker implantation is primarily indicated for patients with symptomatic bradycardia due to sinus node dysfunction or atrioventricular (AV) block, where the heart's intrinsic pacing is insufficient to maintain an adequate heart rate. Conditions such as sick sinus syndrome, complete heart block, and certain cases of second-degree AV block often require pacemakers to prevent syncope and improve cardiac output. Your physician may recommend a pacemaker if you experience persistent fatigue, dizziness, or heart failure symptoms linked to slow heart rhythms.
Indications for ICD Implantation
Implantable Cardioverter Defibrillators (ICDs) are primarily indicated for patients at high risk of sudden cardiac arrest due to life-threatening ventricular arrhythmias, such as those with a history of sustained ventricular tachycardia or fibrillation. ICD implantation is recommended for individuals with reduced left ventricular ejection fraction (typically less than 35%) following myocardial infarction or those with certain inherited arrhythmogenic conditions like long QT syndrome. Your cardiologist will determine ICD candidacy based on these criteria and overall risk of sudden cardiac death.
Risks and Benefits of Pacemakers
Pacemakers regulate abnormal heart rhythms by sending electrical impulses to the heart, reducing symptoms like fatigue and fainting, and improving quality of life for patients with bradycardia or heart block. Benefits include minimally invasive implantation, reliable performance, and a significant decrease in the risk of sudden cardiac arrest associated with slow heart rates. Risks involve infection, device malfunction, lead displacement, and rare complications such as blood clots, emphasizing the importance of regular monitoring to ensure Your safety and optimal device function.
Risks and Benefits of ICDs
Implantable cardioverter-defibrillators (ICDs) provide life-saving interventions by detecting and correcting life-threatening arrhythmias, offering significant benefits for patients at risk of sudden cardiac arrest. Risks associated with ICDs include infection, inappropriate shocks, and device malfunction, which can lead to physical discomfort and psychological stress. Despite these risks, the survival advantage and reduction in sudden cardiac death rates make ICDs a critical option compared to pacemakers, which primarily address slower heart rhythms without defibrillation capabilities.
Pacemaker vs ICD: Which Is Right for You?
Pacemakers regulate slow or irregular heartbeats by sending electrical impulses to stimulate the heart muscle, ideal for bradycardia patients. Implantable Cardioverter Defibrillators (ICDs) monitor heart rhythms for life-threatening arrhythmias, delivering shocks to restore normal rhythm during ventricular tachycardia or fibrillation. Choosing between a pacemaker and ICD depends on individual heart condition severity, arrhythmia risk, and physician's assessment of necessary intervention.
Future Trends in Cardiac Devices
Next-generation cardiac devices integrate advanced AI algorithms for real-time arrhythmia detection and adaptive therapy adjustments, enhancing patient outcomes. Leadless pacemakers and subcutaneous ICDs minimize infection risks and improve battery longevity through wireless charging technologies. Emerging biomaterials and smart sensors enable personalized cardiac monitoring, paving the way for seamless remote patient management and predictive analytics.
Pacemaker vs ICD Infographic
 electrown.com
electrown.com