Urine analyzers provide a quick, non-invasive method to screen for metabolic and kidney disorders by analyzing urine samples, while blood analyzers offer a comprehensive assessment of overall health through detailed blood chemistry and hematology tests. Discover how choosing the right analyzer can impact Your diagnostic accuracy and patient care by exploring the rest of the article.
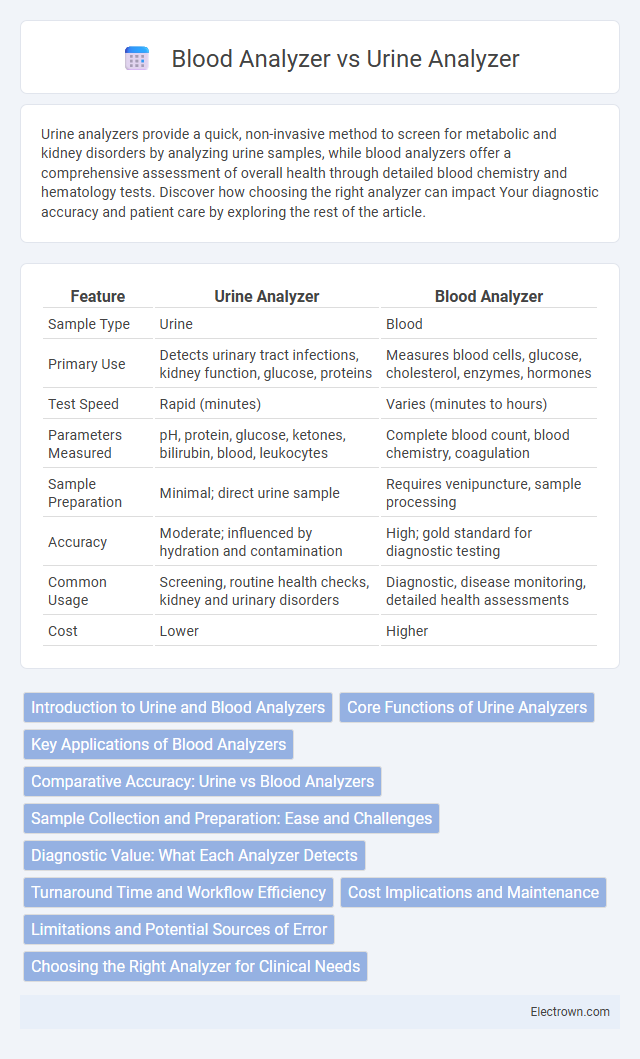
Table of Comparison
| Feature | Urine Analyzer | Blood Analyzer |
|---|---|---|
| Sample Type | Urine | Blood |
| Primary Use | Detects urinary tract infections, kidney function, glucose, proteins | Measures blood cells, glucose, cholesterol, enzymes, hormones |
| Test Speed | Rapid (minutes) | Varies (minutes to hours) |
| Parameters Measured | pH, protein, glucose, ketones, bilirubin, blood, leukocytes | Complete blood count, blood chemistry, coagulation |
| Sample Preparation | Minimal; direct urine sample | Requires venipuncture, sample processing |
| Accuracy | Moderate; influenced by hydration and contamination | High; gold standard for diagnostic testing |
| Common Usage | Screening, routine health checks, kidney and urinary disorders | Diagnostic, disease monitoring, detailed health assessments |
| Cost | Lower | Higher |
Introduction to Urine and Blood Analyzers
Urine analyzers provide rapid, non-invasive testing by examining urine samples to detect infections, kidney function, and metabolic disorders, using advanced dipstick or automated analyzers. Blood analyzers offer detailed insights into your health by measuring blood components such as glucose, hemoglobin, and cholesterol, crucial for diagnosing anemia, diabetes, and cardiovascular diseases. Both analyzers are essential diagnostic tools, complementing each other in comprehensive medical evaluations.
Core Functions of Urine Analyzers
Urine analyzers primarily perform automated analysis of urine samples to detect abnormalities in parameters such as pH, glucose, protein, ketones, and microscopic elements like red and white blood cells. These devices utilize technologies like chemical test strips, flow cytometry, and image analysis to provide rapid, non-invasive screening for urinary tract infections, kidney disease, and metabolic disorders. Their core functions focus on qualitative and quantitative assessments, enabling early diagnosis and ongoing monitoring of patient health through routine urinalysis.
Key Applications of Blood Analyzers
Blood analyzers play a crucial role in diagnosing and monitoring a wide range of conditions including anemia, infections, and blood clotting disorders by providing detailed information on red and white blood cell counts, hemoglobin levels, and platelet function. These devices are essential in managing chronic diseases such as diabetes and cardiovascular disorders by measuring biomarkers like glucose, cholesterol, and cardiac enzymes. Your healthcare decisions rely heavily on the precise data blood analyzers generate to guide treatment plans and assess overall health status.
Comparative Accuracy: Urine vs Blood Analyzers
Blood analyzers provide higher accuracy in detecting systemic conditions due to direct measurement of blood components, offering precise quantification of biomarkers like glucose, cholesterol, and hemoglobin. Urine analyzers are valuable for screening and monitoring metabolic and kidney-related disorders but may have variability influenced by hydration levels and sample handling. Your choice between urine and blood analyzers should consider the specific clinical context and required diagnostic reliability.
Sample Collection and Preparation: Ease and Challenges
Urine analyzers offer the advantage of non-invasive, straightforward sample collection, enabling quick preparation with minimal training, whereas blood analyzers require invasive venipuncture, demanding skilled personnel and careful handling to prevent contamination or clotting. Urine samples are generally easier to procure and process, but their composition varies with hydration and other factors, which can impact analysis accuracy. Your choice depends on balancing ease of collection with diagnostic requirements, as blood samples often provide broader biochemical insights despite the more complex preparation.
Diagnostic Value: What Each Analyzer Detects
Urine analyzers primarily detect metabolic waste products, infections, and kidney function markers such as glucose, proteins, ketones, and leukocytes, providing insights into urinary tract health and systemic conditions like diabetes. Blood analyzers measure a broader range of biomarkers including blood cell counts, electrolytes, enzymes, hormones, and metabolites, offering comprehensive information on overall systemic health, organ function, and disease states. While urine analysis is non-invasive and useful for screening specific conditions, blood analysis delivers detailed diagnostic value critical for detecting anemia, infections, metabolic imbalances, and organ dysfunction.
Turnaround Time and Workflow Efficiency
Urine analyzers typically offer faster turnaround times than blood analyzers due to simpler sample preparation and automated processes, enhancing overall workflow efficiency in clinical settings. Blood analyzers require more complex processing steps, such as centrifugation and staining, which can extend analysis time and reduce throughput. Your choice between these analyzers should consider the balance between rapid results for routine screenings and detailed diagnostics requiring longer processing.
Cost Implications and Maintenance
Urine analyzers generally have lower initial costs and maintenance expenses compared to blood analyzers, making them more accessible for routine diagnostics. Blood analyzers require more frequent calibration, specialized reagents, and skilled technicians, driving up long-term operational costs. Your choice should balance budgetary constraints with the complexity of testing required, as blood analyzers offer more comprehensive data but incur higher maintenance.
Limitations and Potential Sources of Error
Urine analyzers may produce inaccurate results due to sample contamination, improper storage, or patient hydration levels, leading to diluted or concentrated urine that affects readings. Blood analyzers face limitations from hemolysis, clot formation, and improper anticoagulant use, which can cause misleading cell counts or biochemical values. Your diagnostic decisions should consider these potential sources of error to ensure accurate interpretation and reliable clinical outcomes.
Choosing the Right Analyzer for Clinical Needs
Selecting between a urine analyzer and a blood analyzer depends on the specific clinical requirements, as urine analyzers are ideal for detecting metabolic and renal conditions quickly, while blood analyzers provide comprehensive insights into systemic diseases and organ function. Your choice should consider the type of biomarkers needed, sample availability, and diagnostic accuracy essential for effective patient management. Investing in the right analyzer enhances diagnostic precision, streamlines workflows, and supports better clinical outcomes.
Urine Analyzer vs Blood Analyzer Infographic
 electrown.com
electrown.com