Indirect fetal monitoring uses external devices to track your baby's heart rate and uterine contractions without invasive procedures, providing a non-intrusive way to ensure fetal well-being. Understanding the differences between indirect and direct fetal monitoring can help you make informed decisions about your prenatal care; continue reading to learn more about each method's advantages and applications.
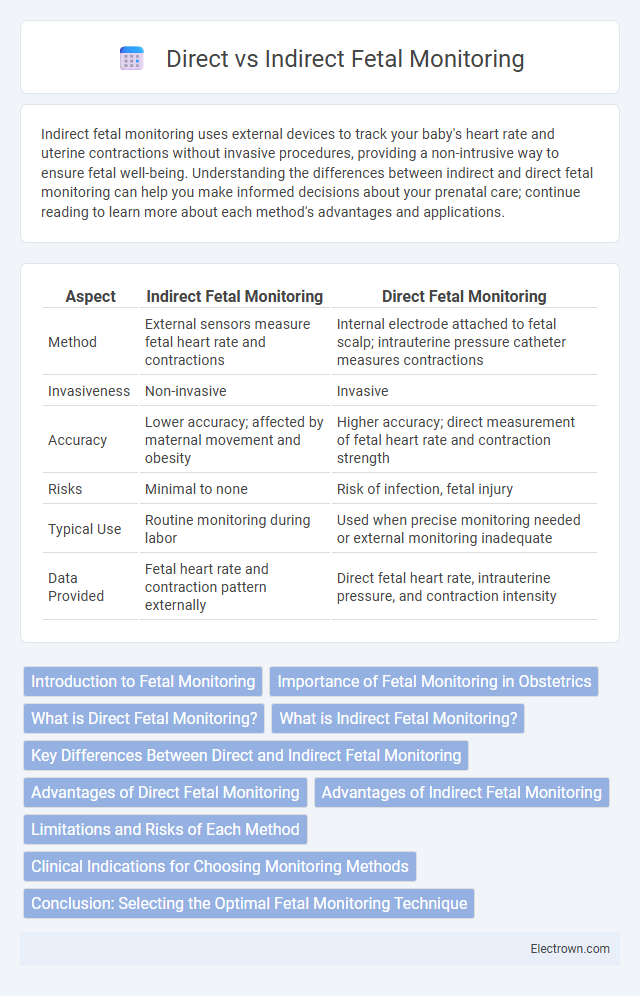
Table of Comparison
| Aspect | Indirect Fetal Monitoring | Direct Fetal Monitoring |
|---|---|---|
| Method | External sensors measure fetal heart rate and contractions | Internal electrode attached to fetal scalp; intrauterine pressure catheter measures contractions |
| Invasiveness | Non-invasive | Invasive |
| Accuracy | Lower accuracy; affected by maternal movement and obesity | Higher accuracy; direct measurement of fetal heart rate and contraction strength |
| Risks | Minimal to none | Risk of infection, fetal injury |
| Typical Use | Routine monitoring during labor | Used when precise monitoring needed or external monitoring inadequate |
| Data Provided | Fetal heart rate and contraction pattern externally | Direct fetal heart rate, intrauterine pressure, and contraction intensity |
Introduction to Fetal Monitoring
Fetal monitoring is essential for assessing your baby's well-being during pregnancy and labor, using either direct or indirect methods. Indirect fetal monitoring, such as external ultrasound and Doppler devices, non-invasively tracks the fetus's heart rate and uterine contractions, offering real-time data without penetrating the amniotic sac. Direct fetal monitoring involves attaching electrodes to the fetal scalp, providing precise and continuous heart rate readings critical during high-risk deliveries for immediate intervention.
Importance of Fetal Monitoring in Obstetrics
Fetal monitoring in obstetrics is crucial for assessing the baby's well-being during labor and delivery, providing real-time data on heart rate patterns and uterine contractions. Direct fetal monitoring, involving a fetal scalp electrode, offers precise and continuous cardiac activity measurement, while indirect monitoring uses external devices like Doppler ultrasound for non-invasive tracking. Your healthcare provider relies on these methods to promptly detect distress, enabling timely interventions that enhance both maternal and fetal safety.
What is Direct Fetal Monitoring?
Direct fetal monitoring involves the placement of an internal fetal electrode on the scalp of the fetus to measure the heart rate accurately. This method provides continuous, real-time data on fetal well-being, especially during labor, by capturing precise cardiac activity signals. It requires rupture of membranes and is typically used when indirect external monitoring poses challenges or when more detailed monitoring is necessary.
What is Indirect Fetal Monitoring?
Indirect fetal monitoring involves assessing the fetus's well-being without direct attachment to the fetus, typically using external devices such as Doppler ultrasound or cardiotocography (CTG) to measure fetal heart rate and uterine contractions through the maternal abdomen. This non-invasive method provides continuous information on fetal heart patterns and uterine activity, allowing early detection of fetal distress during labor. Indirect monitoring is widely used due to its safety, ease of application, and ability to monitor both fetal and maternal parameters simultaneously.
Key Differences Between Direct and Indirect Fetal Monitoring
Direct fetal monitoring involves attaching an internal electrode to the fetus's scalp to record the heart rate precisely, while indirect monitoring uses external sensors placed on the mother's abdomen to detect fetal heart rate and uterine contractions. Direct monitoring provides more accurate and continuous data, especially during labor or high-risk pregnancies, but requires membrane rupture and cervical dilation, unlike the non-invasive indirect method. Your healthcare provider chooses between these based on clinical needs, balancing accuracy with procedure invasiveness.
Advantages of Direct Fetal Monitoring
Direct fetal monitoring provides highly accurate and continuous assessment of the fetal heart rate by using a scalp electrode attached to the fetus. This method offers superior real-time detection of fetal distress compared to indirect monitoring, enabling timely medical interventions during labor. Your healthcare team benefits from precise data that can significantly enhance the safety and outcomes of childbirth.
Advantages of Indirect Fetal Monitoring
Indirect fetal monitoring offers the advantage of non-invasiveness, making it safer for both mother and fetus by avoiding risks such as infection or injury. It allows continuous and long-term monitoring of fetal heart rate and uterine contractions with external sensors, providing valuable information about fetal well-being without causing discomfort. This method is easily accessible, cost-effective, and can be used in various healthcare settings, including outpatient clinics and during early labor stages.
Limitations and Risks of Each Method
Indirect fetal monitoring, such as external Doppler or cardiotocography (CTG), may suffer from signal loss due to maternal obesity, fetal movement, or improper sensor placement, potentially leading to inaccurate or intermittent data. Direct fetal monitoring, which involves placing a fetal scalp electrode or intrauterine pressure catheter, carries risks including infection, membrane rupture, and fetal scalp injury, limiting its use to specific clinical scenarios. Both methods require careful consideration of patient condition and continuous evaluation to minimize risks while ensuring effective monitoring of fetal well-being.
Clinical Indications for Choosing Monitoring Methods
Clinical indications for choosing between indirect and direct fetal monitoring hinge on the risk assessment of maternal and fetal conditions. Indirect fetal monitoring, such as external cardiotocography (CTG), is typically indicated for low-risk pregnancies to non-invasively assess fetal heart rate and uterine contractions. Direct fetal monitoring, including internal fetal scalp electrodes and intrauterine pressure catheters, is reserved for high-risk labor situations requiring precise, continuous data on fetal well-being and uterine activity, especially in cases of labor dystocia or fetal distress.
Conclusion: Selecting the Optimal Fetal Monitoring Technique
Selecting the optimal fetal monitoring technique depends on the clinical context, risk factors, and maternal-fetal condition, as direct fetal monitoring provides more precise and continuous data, especially during labor. Indirect fetal monitoring offers a non-invasive approach suitable for low-risk pregnancies and routine assessments but may lack the accuracy required in high-risk or complicated deliveries. Clinicians must balance accuracy, invasiveness, and patient safety to determine the most effective monitoring strategy for optimal maternal and neonatal outcomes.
Indirect vs Direct Fetal Monitoring Infographic
 electrown.com
electrown.com