Tonometry measures intraocular pressure to assess glaucoma risk, while pachymetry evaluates corneal thickness, influencing tonometry accuracy and treatment decisions. Understanding the differences between these eye tests can help you better interpret your eye health results; read on for a detailed comparison.
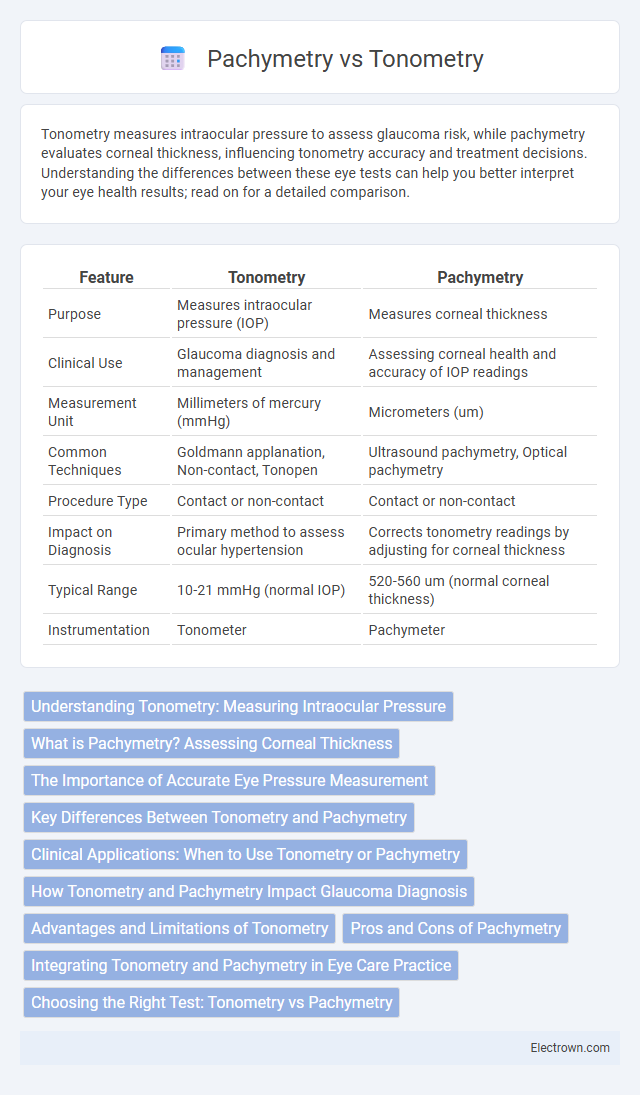
Table of Comparison
| Feature | Tonometry | Pachymetry |
|---|---|---|
| Purpose | Measures intraocular pressure (IOP) | Measures corneal thickness |
| Clinical Use | Glaucoma diagnosis and management | Assessing corneal health and accuracy of IOP readings |
| Measurement Unit | Millimeters of mercury (mmHg) | Micrometers (um) |
| Common Techniques | Goldmann applanation, Non-contact, Tonopen | Ultrasound pachymetry, Optical pachymetry |
| Procedure Type | Contact or non-contact | Contact or non-contact |
| Impact on Diagnosis | Primary method to assess ocular hypertension | Corrects tonometry readings by adjusting for corneal thickness |
| Typical Range | 10-21 mmHg (normal IOP) | 520-560 um (normal corneal thickness) |
| Instrumentation | Tonometer | Pachymeter |
Understanding Tonometry: Measuring Intraocular Pressure
Tonometry is a critical diagnostic procedure used to measure intraocular pressure (IOP), an essential factor in detecting glaucoma and other ocular conditions. This method quantifies the pressure exerted by fluids within the eye, helping ophthalmologists assess the risk of optic nerve damage. Pachymetry, by contrast, measures corneal thickness, influencing the accuracy of tonometry readings by adjusting IOP values based on corneal properties.
What is Pachymetry? Assessing Corneal Thickness
Pachymetry is a diagnostic procedure used to measure corneal thickness, a critical factor in evaluating eye health and diagnosing conditions like glaucoma. Accurate corneal thickness assessment through pachymetry helps determine the risk of glaucoma progression and guides your eye care specialist in tailoring appropriate treatments. Understanding your corneal thickness is essential for precise tonometry readings, as corneal thickness can influence intraocular pressure measurements.
The Importance of Accurate Eye Pressure Measurement
Accurate eye pressure measurement is critical in diagnosing and managing glaucoma, a leading cause of irreversible blindness worldwide. Tonometry directly measures intraocular pressure (IOP), while pachymetry assesses corneal thickness, which can influence IOP readings and lead to misdiagnosis if not accounted for. Combining tonometry with pachymetry ensures precise IOP evaluation, enabling better risk assessment and tailored treatment strategies for preserving vision.
Key Differences Between Tonometry and Pachymetry
Tonometry measures intraocular pressure (IOP) essential for glaucoma diagnosis, while pachymetry assesses corneal thickness, influencing IOP reading accuracy. Tonometers like Goldmann applanation directly gauge eye pressure, whereas pachymeters use ultrasound or optical methods to determine corneal thickness. Understanding your pachymetry results helps interpret tonometry readings precisely, ensuring accurate eye health assessment.
Clinical Applications: When to Use Tonometry or Pachymetry
Tonometry is essential for measuring intraocular pressure, critical in diagnosing and managing glaucoma. Pachymetry evaluates corneal thickness, guiding accurate interpretation of tonometry readings and assessing suitability for refractive surgery. Combining both tests enables comprehensive ocular health assessment, particularly in glaucoma suspects and preoperative evaluations.
How Tonometry and Pachymetry Impact Glaucoma Diagnosis
Tonometry measures intraocular pressure (IOP), a critical risk factor in glaucoma diagnosis, aiding in detecting elevated eye pressure that can damage the optic nerve. Pachymetry assesses corneal thickness, which influences tonometry readings and helps refine the accuracy of IOP measurements. Accurate interpretation of tonometry values combined with pachymetry data leads to more precise glaucoma risk assessment and effective disease management.
Advantages and Limitations of Tonometry
Tonometry offers precise measurement of intraocular pressure (IOP), crucial for diagnosing and managing glaucoma, with non-invasive methods like Goldmann applanation tonometry providing clinical accuracy. However, tonometry's reliability is affected by corneal thickness, curvature, and biomechanical properties, leading to potential IOP measurement errors in patients with abnormal corneas. Unlike pachymetry, which specifically measures corneal thickness to aid in interpreting tonometry results, tonometry alone cannot assess corneal characteristics, limiting its diagnostic scope for comprehensive ocular surface evaluation.
Pros and Cons of Pachymetry
Pachymetry offers precise measurement of corneal thickness, crucial for accurate intraocular pressure (IOP) assessment and glaucoma management, but it requires specialized equipment and trained personnel. It provides direct, reliable data that tonometry alone cannot, especially in patients with abnormal corneal thickness, enhancing diagnostic accuracy. However, pachymetry's invasiveness and cost can limit its routine use in some clinical settings, making it less accessible compared to tonometry.
Integrating Tonometry and Pachymetry in Eye Care Practice
Integrating tonometry and pachymetry in eye care practice enhances glaucoma risk assessment by combining intraocular pressure (IOP) measurement with corneal thickness evaluation. Accurate pachymetry data allows for the adjustment of IOP readings obtained through tonometry, improving diagnostic precision. You can optimize patient care by leveraging both techniques to identify, monitor, and manage ocular hypertension and glaucoma more effectively.
Choosing the Right Test: Tonometry vs Pachymetry
Tonometry measures intraocular pressure (IOP) to screen for glaucoma, while pachymetry assesses corneal thickness, essential for accurate IOP interpretation and refractive surgery candidacy. Choosing between tonometry and pachymetry depends on clinical goals: tonometry for detecting elevated eye pressure and pachymetry for evaluating corneal health and adjusting glaucoma risk assessment. Combining both tests provides comprehensive eye diagnostics, ensuring precise glaucoma management and optimal surgical outcomes.
Tonometry vs Pachymetry Infographic
 electrown.com
electrown.com