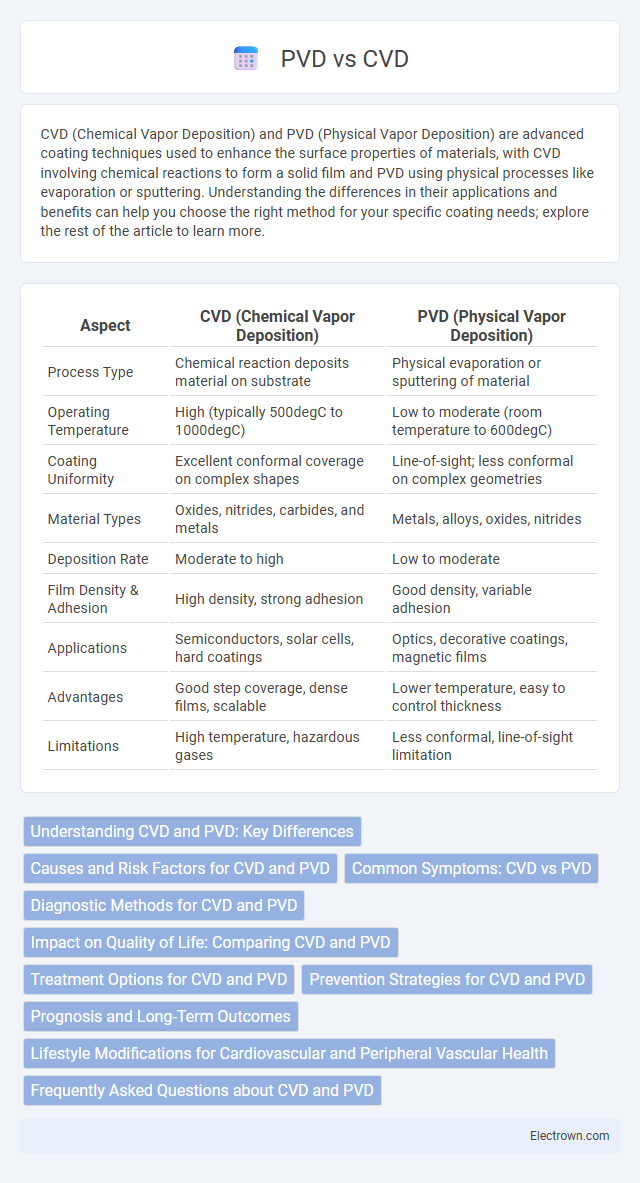
CVD (Chemical Vapor Deposition) and PVD (Physical Vapor Deposition) are advanced coating techniques used to enhance the surface properties of materials, with CVD involving chemical reactions to form a solid film and PVD using physical processes like evaporation or sputtering. Understanding the differences in their applications and benefits can help you choose the right method for your specific coating needs; explore the rest of the article to learn more.
Table of Comparison
| Aspect | CVD (Chemical Vapor Deposition) | PVD (Physical Vapor Deposition) |
|---|---|---|
| Process Type | Chemical reaction deposits material on substrate | Physical evaporation or sputtering of material |
| Operating Temperature | High (typically 500degC to 1000degC) | Low to moderate (room temperature to 600degC) |
| Coating Uniformity | Excellent conformal coverage on complex shapes | Line-of-sight; less conformal on complex geometries |
| Material Types | Oxides, nitrides, carbides, and metals | Metals, alloys, oxides, nitrides |
| Deposition Rate | Moderate to high | Low to moderate |
| Film Density & Adhesion | High density, strong adhesion | Good density, variable adhesion |
| Applications | Semiconductors, solar cells, hard coatings | Optics, decorative coatings, magnetic films |
| Advantages | Good step coverage, dense films, scalable | Lower temperature, easy to control thickness |
| Limitations | High temperature, hazardous gases | Less conformal, line-of-sight limitation |
Understanding CVD and PVD: Key Differences
CVD (Cardiovascular Disease) primarily involves conditions affecting the heart and blood vessels, including coronary artery disease, heart attacks, and stroke, while PVD (Peripheral Vascular Disease) specifically targets the blood vessels outside the heart and brain, often impacting the legs and arms. Risk factors for both include atherosclerosis, smoking, diabetes, and hypertension, but PVD symptoms frequently manifest as leg pain or numbness due to reduced blood flow. Diagnostic methods differ, with CVD assessed through electrocardiograms, stress tests, and angiography, whereas PVD is commonly evaluated using ankle-brachial index measurements and Doppler ultrasound.
Causes and Risk Factors for CVD and PVD
Cardiovascular disease (CVD) and peripheral vascular disease (PVD) share common causes such as atherosclerosis, high blood pressure, and smoking, but PVD specifically involves narrowed arteries reducing blood flow to limbs. Risk factors for CVD include high cholesterol, obesity, diabetes, and sedentary lifestyle, while PVD risk is heightened by similar factors plus age and a history of vascular trauma. Understanding your individual risk factors, including genetic predisposition and lifestyle habits, is crucial for preventing both CVD and PVD.
Common Symptoms: CVD vs PVD
Common symptoms of cardiovascular disease (CVD) include chest pain, shortness of breath, fatigue, and palpitations, often indicating issues with the heart and blood vessels. Peripheral vascular disease (PVD) typically presents with leg pain, cramping, numbness, and slow-healing sores, reflecting reduced blood flow to the limbs. Understanding these symptom differences helps you recognize and seek timely medical evaluation for either condition.
Diagnostic Methods for CVD and PVD
Diagnostic methods for cardiovascular disease (CVD) include electrocardiograms (ECG), echocardiography, stress tests, and coronary angiography, which provide detailed information on heart function and blockages. Peripheral vascular disease (PVD) diagnosis often relies on ankle-brachial index (ABI) measurement, Doppler ultrasound, and angiography to assess blood flow in the limbs. Your healthcare provider may choose specific tests based on symptoms and risk factors to accurately differentiate between CVD and PVD.
Impact on Quality of Life: Comparing CVD and PVD
Cardiovascular disease (CVD) and peripheral vascular disease (PVD) both significantly affect quality of life through symptoms like pain, reduced mobility, and increased risk of serious complications. CVD primarily impacts heart function, leading to fatigue, breathlessness, and limitations in daily activities, while PVD causes poor circulation in limbs, resulting in pain, numbness, and difficulty walking. Managing these conditions early can improve your quality of life by reducing symptoms and preventing progression.
Treatment Options for CVD and PVD
Treatment options for Cardiovascular Disease (CVD) often include lifestyle changes, medications such as statins, beta-blockers, and antiplatelet agents, and surgical interventions like coronary artery bypass grafting or angioplasty. Peripheral Vascular Disease (PVD) management typically involves smoking cessation, exercise therapy, antiplatelet medications, and revascularization procedures including angioplasty or bypass surgery to improve blood flow. Both conditions emphasize risk factor control, but specific interventions vary based on the affected vessels and severity of the disease.
Prevention Strategies for CVD and PVD
Prevention strategies for cardiovascular disease (CVD) and peripheral vascular disease (PVD) emphasize lifestyle modifications such as maintaining a heart-healthy diet rich in fruits, vegetables, and whole grains, regular physical activity, and smoking cessation. Controlling risk factors including hypertension, diabetes, and hyperlipidemia through medication adherence and routine medical monitoring is crucial in reducing incidence rates. Early detection via screening and patient education about symptom awareness further enhance prevention and improve long-term vascular health outcomes.
Prognosis and Long-Term Outcomes
Coronary vascular disease (CVD) often leads to myocardial infarction and heart failure, with prognosis heavily influenced by early intervention and lifestyle modification, resulting in variable long-term outcomes. Peripheral vascular disease (PVD) typically causes limb ischemia and is associated with higher risks of amputation and recurrent hospitalizations, with prognosis dependent on disease severity and management strategies. Both conditions necessitate continuous monitoring to prevent complications, but CVD generally has a higher risk of mortality while PVD more frequently leads to morbidity affecting quality of life.
Lifestyle Modifications for Cardiovascular and Peripheral Vascular Health
Adopting a heart-healthy diet low in saturated fats and rich in fruits, vegetables, and whole grains significantly reduces the risk of cardiovascular disease (CVD) and peripheral vascular disease (PVD). Regular aerobic exercise, such as brisk walking or cycling, improves circulation, lowers blood pressure, and helps manage weight, crucial for preventing both CVD and PVD complications. Smoking cessation and stress management techniques further enhance vascular health by decreasing arterial inflammation and improving endothelial function.
Frequently Asked Questions about CVD and PVD
CVD (Chemical Vapor Deposition) and PVD (Physical Vapor Deposition) are both thin film deposition techniques widely used in semiconductor manufacturing and coating industries. Common questions include their differences in deposition process, with CVD relying on chemical reactions of gaseous precursors and PVD involving physical methods like sputtering or evaporation. Users often inquire about the applications, advantages, and limitations of each method, where CVD typically offers better conformality and PVD provides higher purity and denser coatings.
CVD vs PVD Infographic
 electrown.com
electrown.com